What’s the Role of Myelin Oligodendrocyte Glycoprotein in NMO?
Researchers are working to refine a cell-based assay that more accurately identifies antibodies for myelin oligodendrocyte glycoprotein (MOG) in the serum of patients with neuromyelitis optica spectrum disorders. Some think that anti-MOG-positive patients may even represent a distinct demyelinating disease.
Scientists understand neuromyelitis optica spectrum disorders (NMOSD) far better now than when they were first described as Devic’s disease in 1894. NMOSD is an umbrella category including optic neuritis, myelitis, and acute disseminated encephalomyelitis (ADEM). While researchers understand NMOSD far better than they did even 10 years ago, so much remains obscured.
As we described in our four-part News Synthesis on NMO, researchers and clinicians believed NMO to be a subtype of multiple sclerosis until 2005, when researchers discovered a biomarker for the disease in an antibody that attacks a protein in astrocytes known as aquaporin-4. AQP4 is an integral membrane protein that helps conduct water through the cell membrane. According to Brian Weinshenker, M.D., of the Mayo Clinic in Minnesota, roughly 70% to 80% of adult NMOSD patients test positive for AQP4. Most of them are women.
Unfortunately, anti-AQP4-positive patients usually receive a dire prognosis. Relapses and disabilities are common, while recovery from the attacks tends to be incomplete. The body seems to attack the optic nerves and spinal cord, leading to problems in vision and walking.
 On the other hand, the small subset of NMOSD patients who are seronegative for anti-AQP4 tend to fare better. A small group of labs from Asia and Europe recently confirmed an antibody for myelin oligodendrocyte glycoprotein (MOG) in the sera of some of these anti-AQP4 negative patients. Many of them presented their data at the joint ACTRIMS-ECTRIMS meeting in Boston earlier this month. So far, researchers believe these patients are clinically distinct from the anti-AQP4 patients and may even represent a new disease.
On the other hand, the small subset of NMOSD patients who are seronegative for anti-AQP4 tend to fare better. A small group of labs from Asia and Europe recently confirmed an antibody for myelin oligodendrocyte glycoprotein (MOG) in the sera of some of these anti-AQP4 negative patients. Many of them presented their data at the joint ACTRIMS-ECTRIMS meeting in Boston earlier this month. So far, researchers believe these patients are clinically distinct from the anti-AQP4 patients and may even represent a new disease.
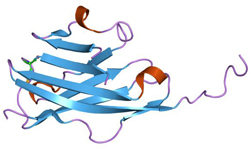
Myelin oligodendrocyte glycoprotein
MOG has captivated and confounded multiple sclerosis researchers for quite some time. The glycoprotein sits atop the outermost layer of myelin, making it an easy target for autoimmune attack. Furthermore, early research demonstrated that a monoclonal antibody (8–18C5) attacked MOG, leading to dramatic demyelination in experimental autoimmune encephalomyelitis mice. The same antibody did not produce similar results in healthy animals. But anti-MOG has a much spottier record in multiple sclerosis, and the jury is still out on whether and how it is involved in demyelination (O’Connor et al., 2007; Mayer and Meinl, 2012). Some think its presence could be a sign of the disease rather than a feature of its pathogenesis. As myelin breaks down, it may expose MOG to the immune system in a novel way, triggering the release of antibodies.
One of the major challenges in studying MOG in humans is that assays for the antibody often lead to nonspecific results and false positives. Traditionally, researchers and clinicians use western blot and ELISA assays to find the MOG antibody, but these assays lead to conflicting results.
In an interview with MSDF, Weinshenker explained that ELISA and western blot assays unfold and stretch out proteins along a gel, making it harder for the antibodies to recognize the protein. “Antibodies recognize conformational epitopes,” he said, “so the protein has to be folded.”
But in 2007, Kevin O’Connor, Ph.D., of Yale University and his team developed a tetramer radioimmunoassay with greater sensitivity to the MOG antibody, an assay that’s highly attuned to MOG’s conformation. This research got the ball rolling on more specific cell-based assays for MOG and helped illuminate its potential role in anti-AQP4-seronegative NMOSD patients.
The cell-based assay
Labs in Japan, Austria, Switzerland, and the United Kingdom are refining and standardizing a cell-based assay for identifying MOG antibodies in NMOSD patients. Douglas Sato, M.D., Ph.D., of Tohoku University in Japan illustrated the basic process of the assay in an email to MSDF. Researchers use human or other mammalian cells to express the MOG antigen on the cell membrane, then expose the cells to diluted serum or cerebrospinal fluid. Then they expose antibody-cell complex to secondary antibodies with fluorescent tags to visualize the complex.
Jacqueline Palace, M.D., of Oxford University and her team are developing several permutations of the assay sensitive to different lengths of MOG. In one study (Kitley et al., 2014), the team found that patients who tested positive for MOG on a short-length cell-based assay generally had a good prognosis. Their attacks were singular events or diagnosed as monophasic NMO.
Palace and her colleagues are also refining a longer-length assay that works similarly to the one Sato described. But she pointed out an important caveat: “If we don’t use a secondary antibody, then we seem to pick up a lot of positives that seem nonspecific.”
Characterizing anti-MOG
Perhaps most importantly, in every study using the cell-based assay, none found overlap between anti-MOG-positive and anti-AQP4-positive patients (Mader et al., 2011; Kitley et al., 2012; Rostásy et al., 2012; Rostásy et al., 2013; Kitley et al., 2014; Mayer et al., 2014; Baumann et al., 2014; Sato et al., 2014). In a commentary published in the same edition of Neurology as Sato et al., Weinshenker (Weinshenker and Wingerchuk, 2014) pointed out two studies that found a total of seven patients positive for both anti-MOG and anti-AQP4. One study using a cell-based assay discovered this dual seropositivity in a single patient (Woodhall et al., 2013); the other study identified the remaining six cases using ELISA staining (Kezuka et al., 2012).
“I firmly believe that’s based on false positives,” Kazuo Fujihara, Ph.D., of Tohoku University said in an interview at the ACTRIMS-ECTRIMS meeting. “MOG is a tricky antigen, and there are many possibilities of false positives.” Fujihara worked with Sato on a study comparing anti-MOG-positive patients to anti-AQP4-positive patients from populations in Japan and Brazil.
All the researchers that MSDF spoke with reported similar clinical characteristics of anti-MOG-positive patients. Generally they make up one-quarter of anti-AQP4-seronegative patients, which accounts for about 5% of the total NMOSD population.
Fujihara said that in his study with Sato, the anti-MOG-positive patients tended to have better outcomes than those who were anti-AQP4-positive. Others said the same of the patients in their studies, and that they generally don’t require treatment since their disease tends to be monophasic. Fujihara noted some important differences between the two groups.
“Firstly, bilateral optic neuritis is quite common in MOG-positive cases, with lesions on both the right optic nerve and the left optic nerve,” he said. “Such lesions are quite rare in AQP4-IgG.” These lesions led to bilateral visual disturbances, which are also seen in anti-AQP4-positive cases, but the lesion distribution was remarkably different.
Fujihara further noted that in anti-MOG-positive cases of myelitis, painful tonic spasm was rare, whereas it’s a common symptom that anti-AQP4-positive patients experience during recovery. Myelitis patients who test positive for anti-MOG also show lesions in the lower portion of the spinal cord, distinct from anti-AQP4-positive patients.
The distribution between men and women who test positive for anti-MOG is also more even. Sato reported that 37% of his sample of 16 were female; Kitley et al. (2014) reported 44% female in a sample of 9.
Of course, the sample sizes remain low, which limits the conclusions researchers can reach.
“To overcome the relative small number of anti-AQP4-seronegative cases in each center, it is important to perform multicenter collaborative studies like ours to increase the number of patients and the number of questions that we can answer with the study,” Sato wrote in an email to MSDF.
Other sources echoed Sato’s sentiment. Kevin Rostásy, M.D., of the Innsbruck Medical University in Austria studies anti-MOG in pediatric NMOSD patients. He said, “It’s an ideal project, certainly for an international collaboration and setup.”
Rostásy’s group found that children with NMOSD have similar clinical phenotypes to adult anti-MOG-positive patients. Like their adult counterparts, they also generally present with a single, dramatic attack that proceeds to a full recovery and no relapses. Unlike adult patients, however, anti-MOG is far more common in pediatric patients, according to Rostásy’s group and data that Anne-Katrin Pröbstel, Ph.D., of the Universität Basel in Switzerland presented at the ACTRIMS-ECTRIMS meeting. Previous work in Pröbstel’s group also found that anti-MOG is only present transiently in the blood of pediatric ADEM patients (Pröbstel et al., 2011).
A new disease?
Palace and others noted the similarity that anti-MOG patients have with the disease that Eugene Devic originally described in 1894. Some sources suggested that anti-MOG-positive patients may represent a new disease.
The evidence for this distinction lies not only in the stark differences in the clinical phenotype between the two groups but also in the fact that there is no overlap between the two groups—at least when researchers use the cell-based assay.
In an interview at ACTRIMS-ECTRIMS, Pröbstel and the principal investigator of her lab, Tobias Derfuss, M.D., were cautious about claiming that anti-MOG-positive patients represented a new disease. However, they did concede that it is possible.
“If it’s really a monoantigen-specific disease, it’s not clear,” Derfuss said. “Why some patients develop MOG and others aquaporin-4, this is not known. You can always speculate about the HLA background, this MHC and no one has quite looked at it.”
Fujihara, on the other hand, seemed more confident. “NMO has been classified as one of the demyelinating diseases, but—based on the findings that I showed you [at the ACTRIMS-ECTRIMS meeting] today—astrocytes rather than myelin seems to be the primary target of NMO.”
“So we are proposing that now NMO should not be classified as a demyelinating disease anymore. AQP4-IgG-positive should be classified as an astrocyte-affecting disease. But on the other hand, MOG-IgG-positive NMO is characterized by demyelinating lesions. So MOG NMOSD are probably demyelinating diseases,” Fujihara said.
Others who spoke with MSDF at ACTRIMS-ECTRIMS seemed to echo that sentiment. In a conversation with MSDF, Hans Lassmann, M.D., of the Medical University of Vienna, Austria, suggested that much of the data in NMOSD is converging on classifying anti-MOG-positive patients as a distinct disease subgroup, owing to its demyelinating pathology.
Lassmann speculated that this could be the first step toward using antibodies like anti-MOG and anti-AQP4 to classify distinct subgroups of diseases that get lumped under the MS category.
“Anti-MOG might pull out another group of patients from the MS lump,” Palace suggested. “Many patients with NMO have been misdiagnosed as MS, and we’ve now pulled them out. And it might be that we pull out another group from the MS pool.”
But, as stated earlier, finding anti-MOG in MS hasn’t been as cut-and-dried. Most sources suggested this was due to the lack of specificity in western blot and ELISA methods. However, Palace said that even with the cell-based assay, she and her colleagues aren’t finding anti-MOG in adult MS patients.
But they do find anti-MOG in some pediatric patients. “We’re not sure whether the children that have it—whether they’ll go on to have true MS or not, or if it’s a different type of the disease.”
To put it simply, researchers need more time to follow up with patients who tested positive for anti-MOG and to gather a larger overall sample.
“I think that this is an evolving story. There seem to be some difference between the group that have MOG versus aquaporin-4 antibody, but the differences are relative, not absolute; they don’t predict those who will relapse versus those who won’t with enough certainty to make clinical decisions," Weinshenker wrote in an email to MSDF. “The data are interesting and potentially clinically important. But, they are not yet ready for clinical testing in order to make a diagnosis, give a prognosis or recommend treatment.”
Though researchers need to continue to work through this question, one thing was obvious to all: International collaboration is key.
Key open questions
- What other antibodies might be biomarkers for disease subgroups?
- Where does the line lie between specificity and usefulness in assays?
- How can these findings be applied to multiple sclerosis patients?
Disclosures and sources of funding
Carol Morton, MSDF’s Senior Science Journalist, contributed to the reporting of this article.
Pröbstel received travel support and is supported by a research fellowship from Genzyme. Her research project is funded by the Swiss Multiple Sclerosis Society and a research grant from the University of Basel.
Derfuss serves on scientific advisory boards for Novartis Pharma, GeNeuro, Octaparma, Merck Serono, Biogen Idec, Genzyme, Mitsubishi Pharma, TEVA Pharma, and Bayer Schering Pharma; has received funding for travel and/or speaker honoraria from Biogen Idec, Novartis, Merck Serono, and Bayer Schering Pharma; and receives research support from the Swiss National Fund, Novartis Pharma, the European Union, and the Swiss MS Society.
Sato’s study received support from KAKENHI (22229008) of the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan, and by the Health and Labour Sciences Research Grant on Intractable Diseases (Neuroimmunological Diseases) from the Ministry of Health, Labour and Welfare of Japan.
Sato receives scholarship from the Ministry of Education, Culture, Sports, Science and Technology (MEXT) of Japan and has received research support from Ichiro Kanehara Foundation.
Fujihara serves on scientific advisory boards for Bayer Schering Pharma, Biogen Idec, Mitsubishi Tanabe Pharma Corporation, Novartis Pharma, Chugai Pharmaceutical, Ono Pharmaceutical, Nihon Pharmaceutical, Merck Serono, Alexion Pharmaceuticals, MedImmune and Medical Review; has received funding for travel and speaker honoraria from Bayer Schering Pharma, Biogen Idec, Eisai Inc., Mitsubishi Tanabe Pharma Corporation, Novartis Pharma, Astellas Pharma Inc., Takeda Pharmaceutical Company Limited, Asahi Kasei Medical Co., Daiichi Sankyo, and Nihon Pharmaceutical; serves as an editorial board member of Clinical and Experimental Neuroimmunology (2009–present) and an advisory board member of Sri Lanka Journal of Neurology; has received research support from Bayer Schering Pharma, Biogen Idec Japan, Asahi Kasei Medical, The Chemo-Sero-Therapeutic Research Institute, Teva Pharmaceutical, Mitsubishi Tanabe Pharma, Teijin Pharma, Chugai Pharmaceutical, Ono Pharmaceutical, Nihon Pharmaceutical, and Genzyme Japan; and is funded as the secondary investigator (22229008, 2010–2015) by the Grants-in-Aid for Scientific Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan and as the secondary investigator by the Grants-in-Aid for Scientific Research from the Ministry of Health, Labour, and Welfare of Japan (2010–present).
Rostásy declared no competing interests and conducts his research with financial support from research grant No. 14158 (KR) of the Jubiläumsfonds of the Austrian National Bank.
Jacqueline Palace is partly funded by highly specialized services to run a national congenital myasthenia service and a neuromyelitis service. She has received support for scientific meetings and honorariums for advisory work from Merck Serono, Biogen Idec, Novartis, Teva, Chugai Pharma, and Bayer Schering, and unrestricted grants from Merck Serono, Novartis, Biogen Idec, and Bayer Schering. Her hospital trust receives funds for her role as clinical lead for the RSS, and she has received grants from the MS society and Guthie Jackson Foundation for unrelated research studies. She is a board member for the charitable European MS foundation The Charcot Foundation and on the steering committee for a European collaborative MS imaging group, MAGNIMS. Her group’s antibody testing is funded by National Health Service National Specialized Commissioning Group for Neuromyelitis Optica and the National Institute for Health Research Oxford Biomedical Research Centre.
Weinshenker declared no competing interests.


