New MS Clinical Course Descriptions Reflect Disease Activity
Refined descriptors for the course of MS, replacing those in use since 1996, are intended to make communication with patients clearer and to enhance the design and conduct of clinical trials
The International Advisory Committee on Clinical Trials in Multiple Sclerosis (MS) has issued refined descriptors for MS course that include disease activity based on clinical relapse rate and MRI, as well as disease progression. The revised 2013 definitions, intended to replace those in use since 1996, were published online ahead of print May 28 in Neurology (Lublin et al., 2014).
“As time went on since 1996, we understood more of the biological underpinnings of MS and wanted to incorporate these in new definitions,” second author Stephen C. Reingold, Ph.D., told MSDF. “In 2011, we had an international conference to revisit what we had done 18 years ago. The previous definitions are basically appropriate, but it is important to consider clinical or MRI activity or disability over a shorter time frame, and the new definitions now incorporate these measures.”
A survey of international MS experts resulted in the 1996 clinical course descriptions, or phenotypes, based on purely clinical data and consensus opinion available at that time. Because neuroimaging and biological measures were still lacking in 1996, the International Advisory Committee became concerned that the original descriptors may incompletely reflect more recently identified clinical aspects of the disease, as well as advances in understanding the underlying pathology.
The refined phenotype descriptions developed in 2013 therefore include more accurate clinical descriptive terminology, MRI and other imaging markers. The panel considered cerebrospinal fluid biomarkers and neurophysiological measures but chose not to include them in their descriptors.
“Our goal for modifying the 1996 definitions is to better characterize patients with MS and provide a framework for both clinical research and ongoing clinical care,” lead author Fred D. Lublin, M.D., FAAN, FANA, told MDSF. Lublin is the Saunders Family Professor of Neurology and director of the Corinne Goldsmith Dickinson Center for Multiple Sclerosis, Icahn School of Medicine at Mount Sinai, New York, NY. “These revisions should make communication with patients and among physicians clearer and should also enhance the design, recruitment, and conduct of clinical trials, which will further help us understand the disease.”
Research since 1996 has yet to identify imaging and biological markers that might provide objective criteria for distinguishing clinical phenotypes. Nonetheless, the International Advisory Committee proposed refined descriptors including measures of clinical relapse rate, imaging findings, and disease progression to reflect overall MS activity.
“The new descriptors incorporate what has been learned regarding the increased sensitivity of MRI in detecting MS disease events to more accurately capture the activity of the disease,” Bruce A. Cohen, M.D., told MDSF when asked for independent comment. Cohen is a professor in the Davee Department of Neurology and Clinical Neurosciences at Northwestern University Feinberg School of Medicine and director of the Northwestern Comprehensive Multiple Sclerosis Program in Chicago, Illinois. “The use of the term ‘activity’ adds clarity to the prior need to extend the characterization of relapsing types of MS in order to incorporate MRI data.”
The 2013 International Advisory Committee also recommended strategies for future research to develop more refined phenotype definitions, which should further enhance treatment decisionmaking.
Changes in clinical course descriptions
The 1996 clinical course descriptions included standardized definitions for four MS clinical courses representing the spectrum of clinical MS subtypes: relapsing-remitting (RR), secondary progressive (SP), primary progressive (PP), and progressive relapsing (PR). However, the experts who developed these descriptions acknowledged the need for change over time as better imaging modalities and biomarkers became available.
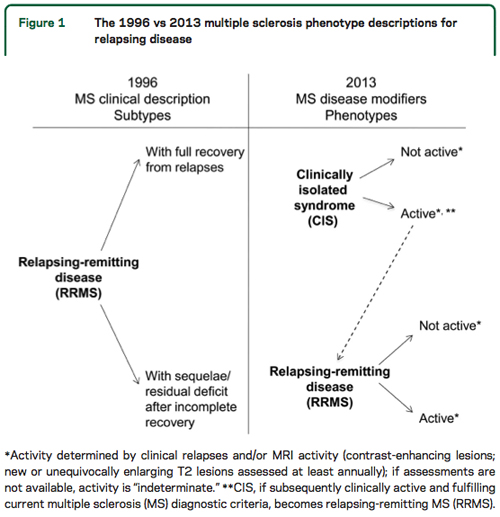
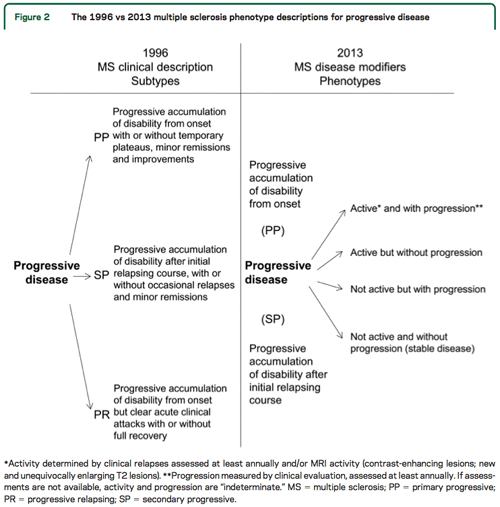
The revised 2013 descriptions retain the core MS phenotype descriptions of relapsing and progressive disease, with some modifications intended to reflect ongoing inflammatory or neurodegenerative disease. The goal of the revised descriptions is to facilitate prognosis, therapeutic decisions, and clinical trial designs and outcomes.
Additional meaningful descriptors of both relapsing and progressing disease include disease activity identified from clinical relapses, from progression of disability, or from MRI measures of gadolinium-enhancing lesions or new or definitively enlarging T2 lesions.
“The revision of the term ‘progressive disease’ and the linkage to observation time, and the distinction of worsening active disease from relapse activity from gradual disability progression, are important terminology clarifications which reflect experience with current therapeutics and possible changes in natural history in the therapeutic era,” Cohen said. “These will be important considerations in clinical trial design and analysis, and also in evaluating therapeutic effects at the individual level.”
Specific recommendations for evaluation and classification
- Persons with relapsing MS should undergo clinical evaluation and brain MRI at least annually.
- Persons with progressive MS should undergo annual clinical evaluation, but there was no consensus among committee members regarding the optimal frequency of brain imaging. However, they did recommend that progression be determined annually by history or objective measure of change.
- In the absence of spinal clinical findings, annual spinal cord imaging is not recommended.
- The existing course descriptions should be subcategorized based on activity or progression. Someone with RRMS and a new gadolinium-enhancing lesion on MRI would be classified as RR-active, whereas someone with RRMS and no relapses or enlarging or new MRI lesions during the evaluation period would be classified as RR-not active.
“These criteria will emphasize the need for high-quality regular MRI as an important tool for evaluating disease course in MS, provided that procedures and mechanisms can be implemented into clinical practice settings to ensure that imaging is done with sufficient quality to allow serial analysis to be accurate,” Cohen said.
- Because activity is included as a modifier of basic clinical course phenotype, the PR category can be eliminated, the committee decided. Someone with PPMS who has an acute attack would now be classified as PP-active.
- To date, insufficient evidence supports the use of cerebrospinal fluid biomarkers, optical coherence tomography, or evoked potentials in clinical MS descriptors.
- The revised MS phenotype descriptors include clinically isolated syndrome (CIS), which was not included in the 1996 descriptors. CIS is thought to be the first clinical presentation of inflammatory demyelination that could be MS. Persons with CIS should be prospectively followed to identify their subsequent MS phenotype.
- In contrast, the committee decided that radiologically isolated syndrome, characterized by incidental imaging findings consistent with inflammatory demyelination in asymptomatic persons, should not be considered a separate MS phenotype.
- Benign and malignant MS, as described by consensus, are not MS phenotype descriptors in and of themselves, but they may give an indication of disease severity over time.
- Worsening disease refers to a documented increase in neurologic dysfunction and/or disability due to relapses or progressive disease.
Likely acceptance of new MS descriptors
“The prior course definitions we published in 1996 were widely adopted,” said Lublin, who was part of that panel and who is also co-chief editor of Multiple Sclerosis and Related Disorders. “As the current recommendations were a consensus of 32 MS experts and journal peer review, I do not expect much controversy, but time will tell.”
Features of the new recommendations that should facilitate their acceptance, according to Cohen, are “their enhanced clarity in describing MS as we currently understand it, and their consistency with what we have learned in the interval since the 1996 phenotypes were adopted.”
Reingold, who is president of Scientific and Clinical Review Associates, LLC, noted that the 1996 definitions were well received and quickly implemented in clinical trials, and that it was very easy to reach consensus in the group that developed the new definitions.
“There was some concern regarding the recommendation for annual MRI in terms of healthcare costs and also in that MRI lesions may not always reflect clinical changes,” Reingold said. “Currently, most clinicians often use MRI only if the patient is doing worse. We waffled a little and said that clinicians could use MRI more or less frequently, but that they should document the frequency and their underlying reasons.”
Potential impact of new MS descriptors
“If the MRI shows new gadolinium-enhancing lesions when there is no clinical change, we might consider starting or switching therapy,” Reingold said. “In terms of clinical trials, we should include measures of activity and consider stratification based on these measures. This could help determine whether a new therapy works on all forms of MS, or only on active or inactive MS.”
Cohen agreed that better stratification of participants in clinical research should help to refine our understanding of clinical therapeutic regimens and their impact.
In terms of additional research, Lublin recommended long-term longitudinal and cohort studies, imaging studies, prospective follow-up, and research to better understand and define MS phenotypes. These should continue to refine the framework for clinical research and improve clinical care and decisionmaking.
“From the clinical standpoint, more than anything else, we need robust markers of MS activity which are affordable, reliable, and sensitive enough to be used at the individual level to robustly predict disease activity, therapeutic response, and disability prognosis,” Cohen concluded. “At the research level, we need to understand the pathologic mechanisms underlying these phenotypes and their relationship to each other, more sensitive tools to detect these pathological mechanisms in vivo, and a better understanding of the causative factors which initiate and sustain the disease.”
Key open questions
- How will future research further refine MS clinical descriptors incorporating objective measures of disease activity?
- How will the new descriptors be accepted and implemented, and what will be their impact on research trials and clinical practice?
Disclosures and sources of funding
The many authors of the Neurology article reported various disclosures involving pharmaceutical companies, as described in the online article. Dr. Cohen did not report any financial disclosures.


