No Causal Link Found Between Vaccines and MS
A large case-control study showed no causal link between current vaccines and the risk of MS or other CNS demyelinating disease, but there was a short-term increased risk in younger patients
A large nested case-control study, published October 20 in JAMA Neurology, showed no causal link between current vaccines and the risk of multiple sclerosis (MS) or other acquired demyelinating syndromes affecting the CNS (CNS ADS) (Langer-Gould et al., 2014). However, there was a short-term increased risk in younger patients, which the authors suggest most likely represented preexisting, asymptomatic disease revealed by the antigenic stimulus of vaccination.
 “The concern that vaccinations could induce a small increased risk of [MS] and other [CNS ADS] remains controversial,” wrote Annette Langer-Gould, M.D., Ph.D., from the Department of Research and Evaluation, Kaiser Permanente, Southern California in Pasadena, and colleagues. “… Because vaccinations are common, even a small increased risk of [MS] or other [CNS ADS] could have a significant effect on public health.”
“The concern that vaccinations could induce a small increased risk of [MS] and other [CNS ADS] remains controversial,” wrote Annette Langer-Gould, M.D., Ph.D., from the Department of Research and Evaluation, Kaiser Permanente, Southern California in Pasadena, and colleagues. “… Because vaccinations are common, even a small increased risk of [MS] or other [CNS ADS] could have a significant effect on public health.”
Previous studies of the association between vaccination and risk for MS have shown mixed results. Most studies did not find any association, and the remainder had limitations including small sample size. There are some case reports of young women with acute CNS symptoms within 1 month of vaccination, suggesting that the vaccine may accelerate the transition from subclinical to clinical disease.
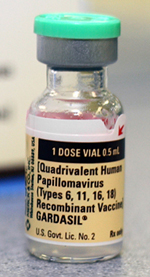
The study goals were to identify or rule out an association between use of vaccines, particularly those for hepatitis B (HepB) and human papillomavirus (HPV), and risk of MS or other CNS ADS, over the long and short term.
Using the complete electronic health records of Kaiser Permanente Southern California members, the investigators identified cases through the KPSC CNS ADS cohort between 2008 and 2011, as well as five controls per case, matched for age, sex, and zip code.
Available data on the cases included extensive review of medical records by an MS specialist. The electronic vaccination records system allowed identification of vaccination of any type for cases and controls. Use of conditional logistic regression allowed adjustment of any associations for race/ethnicity, healthcare utilization, comorbid conditions, and infectious diseases before onset of symptoms.
Among 780 cases of CNS ADS and 3885 controls, there were 92 cases and 459 controls who were females aged 9 to 26 years (the indicated age range for HPV vaccination). The analysis did not identify any associations between vaccination and the risk of CNS ADS up to 3 years later. For HepB vaccination, the odds ratio (OR) for risk of CNS ADS was 1.12 (95% CI, 0.72-1.73). For HPV vaccination, OR was 1.05 (95% CI, 0.62-1.78), and for any vaccination, OR was 1.03 (95% CI, 0.86-1.22).
However, vaccination of any type was associated with more than twice the risk of CNS ADS onset within the first 30 days after vaccination, but only in persons under 50 years of age (OR, 2.32; 95% CI, 1.18-4.57). The increase in absolute risk was small, however. Among the cases, 4.1% acquired a CNS demyelinating syndrome compared to 2.5% of controls.
“We found no longer-term association of vaccines with MS or any other CNS ADS, which argues against a causal association,” the study authors wrote. “The short-term increase in risk suggests that vaccines may accelerate the transition from subclinical to overt autoimmunity in patients with existing disease.”
Study limitations include insufficient power to detect associations with rare forms of CNS ADS; uncommon exposures such as use of single-antigen HepB vaccine or HepB vaccination in early childhood; vaccine preservatives; and subgroups including older persons, those with genetic predisposition, or young women with symptom onset within 180 days following HPV vaccine.
“Our findings support clinical anecdotes of CNS ADS symptom onset shortly after vaccination but do not suggest a need for a change in vaccine policy,” the study authors concluded.
Key open questions
- What would further epidemiological studies disclose regarding any associations of HPV or HepB vaccination, overall and in subgroups, with MS or other CNS ADS?
- What, if any, cost-effective strategies could be devised to identify persons at risk for acute symptom onset after vaccination and to prevent these symptoms without interfering with vaccine efficacy?
Disclosures and sources of funding
Kaiser Permanente Direct Community Benefit Funds and the National Institute of Neurological Disorders and Stroke supported this study. Some of the study authors reported various financial disclosures involving Biogen Idec, Hoffmann-LaRoche, National Institutes of Health, National MS Society, research funding for studies related to HPV vaccine, and/or research funding from Novartis for studies unrelated to this research.



Comments