Physical Activity Associated With Improved Quality of Life in People With MS
An international survey of over 2000 people with MS shows that moderate to high levels of physical activity are associated with better health-related quality of life

Physical activity is highly associated with better quality of life in people with MS, according to a large international survey published in BMC Neurology (Marck et al., 2014). While the physical and psychological benefits of exercise are well known in healthy communities, researchers continue to debate whether the same benefits exist for people with MS. One of the biggest barriers to exercise for MS patients is fatigue, and many feel that avoiding exercise will help maintain energy. Balance and coordination issues also diminish the motivation to exercise.
The current study surveyed 2232 people with MS, recruited through online MS societies and social media platforms. Participants completed a 40-minute questionnaire and recorded their contact information for follow-up studies.
The researchers collected data on each participant’s height, weight, age, and gender. They quantified physical activity using the International Physical Activity Questionnaire that measures self-assessed physical activity as well as sitting time over the past 7 days. They then divided the responses into three categories of high, moderate, and low activity.
Finally, the team assessed each participant’s degree of disability using the patient-determined disease steps (PDSS), a tool for patients to self-determine their own level of disability. Scores can range from 0 (normal) to 8 (bed bound). However, the researchers condensed the data into three categorical variables. Scores of 0 to 2 were considered low disability, 3 to 5 moderate disability, and 6 to 8 high disability.
The dependent variables in the study included the physician-diagnosed relapse rate, determined over the previous 12 months. For participants with relapsing-remitting MS (RRMS), the researchers measured the relapse rate over the prior 5 years. The researchers also assessed disease activity in participants with RRMS and categorized it as increasing, decreasing, or stable.
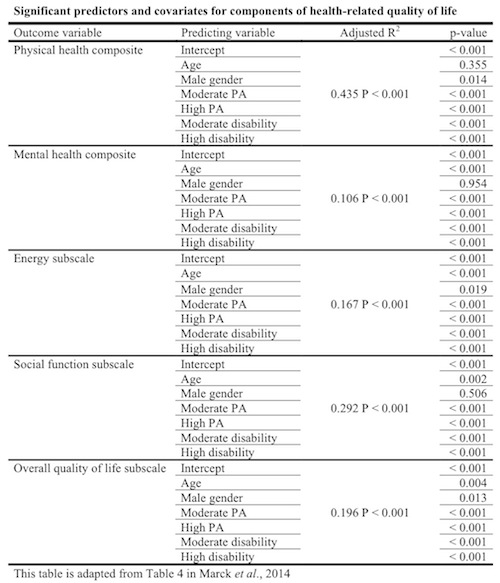
The team also looked at how physical activity affected body mass index and health-related quality of life (HRQOL). They measured HRQOL using the 54-item MS Quality of Life (MSQOL-54) survey.
The results
Unsurprisingly, lower levels of physical activity were associated with increasing disability. More than 80% of people in the high-disability group fell into the “low physical activity” category, though only 37% of people in the low-disability group practiced a high level of activity. The remaining 63% of the low-disability group were either moderate or low exercisers, with 36.5% practicing moderate activity, and the remaining 26.5% exercising little.
Physical activity also correlated with gender, age, and BMI. Males were generally more active than females, but that difference only reached statistical significance in the low-disability group. As one may expect, older participants were generally less active than younger, and participants with higher BMI scores were less active than those with lower scores as well.
The researchers initially found that relapse rates in people with RRMS were higher in the low-activity group. Even participants who practiced a moderate amount of physical activity had fewer relapses. However, once they controlled for age, gender, disability, and physical activity, they found no significant relationship between physical activity and relapse rate. The researchers also did not find any correlation between disease activity and physical activity levels.
The researchers found that physical activity and quality of life were highly associated with each other. In all subscales of the MSQOL-54, quality-of-life scores were positively associated with increased physical activity. The only exception was in mental health scores, where there was no significant difference between moderate and high physical activity.
Even after controlling for age, gender, and disability in the regression model, the researchers found that the association between physical activity and quality-of-life subscales still reached statistical significance. The following table summarizes the results.
Implications
This study represents a growing movement toward advising people with MS to engage in physical activity. Even moderate activity, defined in this study as walking for at least 20 minutes 3 days per week, correlated strongly with high quality-of-life scores for people with MS.
The researchers mentioned that physical activity in a group setting, such as a team sport, may help social functioning in people with MS. On the other hand, a self-initiated solitary activity, like running, may lead to higher feelings of self-efficacy.
In the paper, the authors said that the evidence for the benefits of exercise is accumulating, and physicians may begin encouraging their patients to exercise instead of recommending they avoid it.
Key open questions
- What are the best exercises for patients with moderate to high levels of disability?
- Is it possible that physical activity may also help reverse or slow the progression of MS?
Disclosures and sources of funding
Marck and her co-authors received funding for this study from the Bloom Foundation and the Horne Family Charitable Foundation. One of the authors, George Jelinek, receives royalties from his book, Overcoming Multiple Sclerosis: An Evidence-Based Guide to Recovery.



Comments
Barbara Giesser, M.D., UCLA
Though these findings aren’t necessarily new, the biggest strength of this study is the large sample size. The drawback is that all the data is self-reported and it’s hard to verify whether someone who says they exercise three times a week is being accurate. However, the take-home message is that exercise is good for people with MS. Not only does it help overall fitness and well-being, but also there is evidence that exercise is important in managing comorbidities such as diabetes and hypertension. This is because studies indicate that people with MS who have such coexisting conditions have worse neurologic outcomes.
Some data from animal models also show that physical activity is good not just for muscles but for nerves as well. In animals, exercise has been shown to improve dendritic growth and nerve density, as well as promote the expression of anti-inflammatory proteins. Exercise has been shown to ameliorate the animal model of MS. Other studies have reported that people with MS who exercise have improvement in symptoms such as fatigue and depression. There’s also some new evidence that exercise can improve cognitive impairments as well.
Ultimately, this study shows that we no longer need to be afraid of encouraging patients with MS to exercise. In fact, we should encourage it, along with tips on how to avoid overheating.
References:
PMID 24999244. Klaren RE, Motl RW, Woods JA, Miller SD.
PMID 24158978. Briken S, Gold SM, Patra S, Vettorazzi E, Harbs D, Tallner A, Ketels G, Schulz KH, Heesen C.