Can Gut Microbes Provide Answers About MS?
Is the gut as interesting as the brain? Researchers probing the ecosystem of the human gut microbiome have identified organisms that are enriched or depleted in MS patients, possibly yielding clues about pathogenic mechanisms. Meanwhile, introducing a nonhuman pathogen into the gut is being investigated as a possible treatment approach.
“I am going to argue that the gut is as interesting as the brain,” said Sushrut Jangi, M.D., an internist working in the laboratory of Howard Weiner, M.D., at Brigham and Women’s Hospital in Boston. Jangi was speaking at the American Academy of Neurology (AAN) annual meeting in Philadelphia on April 30, 2014, about the gut microbiome of multiple sclerosis (MS) subjects.
The human gut is populated by an entire ecosystem of microbes that plays a crucial role in regulating many physiological processes, notably both innate and adaptive immune responses. According to Jangi, the relationship between the microbiome and the immune system is most clearly seen in autoimmune models. For example, transgenic experimental autoimmune encephalomyelitis mice are protected against disease when raised in germ-free conditions but become susceptible when researchers introduce commensal gut bacteria.
Jangi and colleagues were interested in whether the gut ecosystem in patients with MS differs from that seen in healthy controls. They collected fecal samples from 168 relapsing-remitting MS (RRMS) patients and 77 healthy controls. Then they sent 61 MS samples and 43 control samples for high-throughput sequencing to determine the composition and structure of the gut microbiome.
The team assessed two different types of diversity: alpha diversity, which is a measure of diversity within the ecosystem; and beta diversity, a measure of dissimilarity between ecosystems. They found that MS patients and healthy controls had similar levels of both alpha and beta diversity.
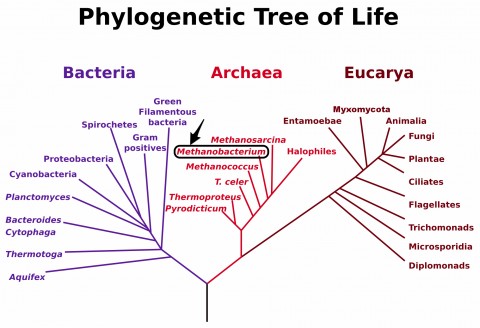
However, at a species level, they saw marked differences. First, they found that an organism called methanobrevibacteriaceae is significantly increased in MS patients compared to healthy controls, whether or not patients were treated. This particular bug is a member of the Archaea kingdom, which is distinct from the bacteria and eukaryotes found in the gut. Although the microbe is present in only about 50% of MS patients, when it’s there, levels are about 10- to 50-fold higher than in healthy controls. Moreover, MS patients highly enriched for methanobrevibacteriaceae had significantly increased Expanded Disability Status Scale (EDSS) scores compared to those not enriched for the bug (EDSS scores of 1.85 and 1.1 respectively, p = 0.036) and tended to have a longer disease duration.
Interestingly, methanobrevibacteriaceae are also found in obese individuals and those with inflammatory bowel disease, and in mouse models have been linked to the induction of inflammation. Jangi and colleagues coincubated peripheral blood mononuclear cells with different dilutions of methanobrevibacteriaceae and showed a dose-related proliferation of the PBMCs and induction of proinflammatory cytokines regardless of whether the cells came from MS patients or healthy controls.
They also found that two other organisms were depleted in MS patients but increased in patients receiving MS treatment. Both of these organisms—one from the Butyricimonas genus (phylum: Bacteroidetes) and one from the Lachnospiracaea family (Firmicutes phylum)—have anti-inflammatory effects, presumably the result of their increased production of the short-chain fatty acid butyrate, which boosts the generation of regulatory T cells.
According to Scott Peterson, Ph.D., a microbiome researcher at Sanford-Burnham Medical Research Institute in La Jolla, California, who was not involved in this study, these associations between MS and certain bacterial species are in line with what other microbiome research has shown but a long way from establishing causality. “If you lumped all the diseases together in which the microbiome has been implicated, we are starting to see causality being established,” he told MSDF. “With autoimmunity, I don’t know of examples yet where causality has been established. But with both diabetes and MS, I am becoming convinced that the gut microbiome can modulate the severity of those disease types. Whether or not they are initiators or perpetuators, or something in between, is far less clear.”
Gut worms may also play a role
Despite the fact that research on the human microbiome is still in its early stages, there are already efforts to manipulate the microbial ecosystem in the gut as a means of treating diseases, including MS. One of the implications of our improved understanding of the gut microbiome is that it provides evidence to support the “hygiene hypothesis,” which posits that improved hygiene, resulting in reduced exposure to microbes and less frequent early childhood infections, could contribute to an increased incidence of allergic and immunologic illnesses. In 2007, Jorge Correale, M.D., and Mauricio Farez, M.D., demonstrated that MS patients with parasite infections had not only decreased exacerbations and fewer MRI lesions than uninfected patients, but also increased induction of regulatory T cells (Correale and Farez, 2007).
 Might intentional exposure to these parasites offer protection against disease? That’s the idea behind several clinical trials now underway around the world. John Fleming, M.D., a neurologist at the University of Wisconsin School of Medicine and Public Health, presented early results at the AAN annual meeting from one such trial of the helminth Trichuris suis ova (TSO), more commonly known as porcine whipworm, in patients with RRMS.
Might intentional exposure to these parasites offer protection against disease? That’s the idea behind several clinical trials now underway around the world. John Fleming, M.D., a neurologist at the University of Wisconsin School of Medicine and Public Health, presented early results at the AAN annual meeting from one such trial of the helminth Trichuris suis ova (TSO), more commonly known as porcine whipworm, in patients with RRMS.
This phase 2 clinical trial of helminth-induced immunomodulation therapy (HINT) enrolled 15 recently diagnosed, treatment-naive RRMS subjects. After an initial 5-month observation period (so that subjects could serve as their own controls), each subject received a dose of 2,500 TSO in liquid form every two weeks for 10 months, followed by 4 months of posttreatment observation. Investigators conducted brain MRI scans with gadolinium contrast, immunological assessments, examination of stool samples, and EDSS assessments at multiple times throughout the study.
EDSS scores averaged 1.3 ± 0.9 at screening and 1.5 ± 0.9 after TSO treatment; this was associated with a nonsignificant relative reduction of 36% in active (gadolinium-enhancing) MRI lesions. Four patients relapsed during the study. Half of the subjects had mild, transient gastrointestinal symptoms about 30 days after the first TSO dose.
Investigators conducted exploratory mechanistic studies on subsets of subjects. These studies showed an increase in Tregs and a decrease in expression of the Peli1 gene, a regulator of microglial inflammation. An analysis of stool samples from a subgroup of MS HINT subjects before or after treatment, as well as MS controls and healthy controls, showed no statistically significant changes in the bacterial community populations among these different populations.
According to Fleming, these preliminary results suggest that further investigation of helminth therapy is warranted, although it’s too early to say whether there is a place for helminth therapy among the many MS therapies currently on the market or in development. “The idea of a parasite is of course an unusual one for therapy—there’s the ‘yuck factor,’ ” he told MSDF. “However, when the rationale and safety provisions are explained, research subjects were quite comfortable with this probiotic agent.”
Two other helminth-based clinical trials are currently underway, one of them at the University of Nottingham in the U.K. This trial, WiRMS (Worms for Immune Regulation in Multiple Sclerosis), uses a hookworm larvae, Necator americanus, rather than TSO. Lead researcher Cris Constantinescu, M.D., Ph.D., cited several advantages to this approach in an email to MSDF: “It is a strictly human parasite and the infection is a one-off, with the subject remaining infected for the lifespan of the hookworm (5 years) or until the parasite is killed with anti-helminthics.” In addition, he said that the hookworm is guaranteed to remain in the gut, while some other parasites have been known to migrate outside of the gut.
Fleming agreed that there may be advantages to using a human pathogen. There is also the possibility that once RRMS has been established, helminth exposure may be too late to be efficacious. Further study of the mechanisms may provide clues about the effects of helminth exposure and the relationship of helminths with other residents of the gut microbiota. “We are all of the sudden presented with this ability to enumerate a thousand microbes in the gut and when it comes right down to it we know very little about their biochemistry and what proteins and metabolites they make,” Peterson said.
Key open questions
- What is the temporal relationship between changes in prevalence of certain microbial species and disease progression in MS?
- Can the microbiome of a person with MS be altered to more closely resemble that of a healthy person, and if so, what effect does that have on the disease course?
- How long-lasting are the immunomodulatory effects of helminth treatment?
Disclosures and sources of funding
Dr. Jangi’s study was supported by the NIH and a pilot grant from the National Multiple Sclerosis Society. Dr. Jangi had nothing to disclose. Dr. Weiner has received personal compensation for activities with Biogen Idec, Novartis, EMD Serono, Teva Neuroscience, GlaxoSmithKline Inc., Nasvax, Xenoport Inc., and Genzyme Corp. Dr. Weiner has received research support from Merck Serono. Among their co-authors, one has received research support from Merck Serono, and another has received personal compensation for activities as a consultant, scientific adviser, and speaker. The HINT study is supported by a National Multiple Sclerosis Society Research Grant and the National Institutes of Health.
Dr. Fleming had nothing to disclose. One of his co-authors has received personal compensation for activities with Biomarin, GlaxoSmithKline Inc., Zensun, Neuraltus, Merck & Co. Inc., and Adventrx.
Dr. Peterson had nothing to disclose.
Dr. Constantinescu has received personal compensation for activities with Biogen Idec, Teva Neuroscience, and Novartis, and he has received research support from Serono Inc., Biogen Idec, Teva Neuroscience, and Novartis.


