The Many Faces of B Cells
Experimental therapy prompts a closer look at immune cells
Five years ago, just as the global economy plummeted, interest in B cells spiked upward among multiple sclerosis (MS) researchers. The trigger was the published report that the anti–B cell drug rituximab significantly reduced relapses and new brain lesions in a phase 2 clinical trial of 104 people with relapsing-remitting MS (RRMS) (Hauser et al., 2008).
 Until then, B cells were assumed to be stoking MS mainly by pumping out antibodies and priming CD4+ T cells to attack the myelin wrapper around neurons in the brain and spinal cord. Now, researchers are investigating other ways B cells may be involved in MS and the therapeutic implications (see "B Cells Step Into the Limelight").
Until then, B cells were assumed to be stoking MS mainly by pumping out antibodies and priming CD4+ T cells to attack the myelin wrapper around neurons in the brain and spinal cord. Now, researchers are investigating other ways B cells may be involved in MS and the therapeutic implications (see "B Cells Step Into the Limelight").
A session at the recent meeting of the Federation of Clinical Immunology Societies (FOCIS), in Boston, Massachusetts, offered a sample of B-cell research that bridged basic and clinical immunology, including experimental new translational therapies for MS. The discussion about the therapeutic potential of targeting B cells will continue at a satellite symposium at the European Committee for Treatment and Research in Multiple Sclerosis (ECTRIMS), to be held October 2–5, 2013, in Copenhagen, Denmark.
"T cells are probably still considered the master orchestrators, but T cells and B cells are highly dependent upon each other," panelist Joan Goverman, Ph.D., an immunologist at the University of Washington, Seattle, told MSDF in an interview after the FOCIS meeting. T cells are the immune troops that need to be near the action to be effective, whether it is killing an offending cell or instructing other immune cells. B cells are best known as the remote drones of the immune system, able to unleash quick-acting, wide-ranging antibodies, but only after one-on-one confirmation from a CD4+ T cell. That requires the B cell to assume another role, as an antigen-presenting cell, Goverman said. The consultation may spur a B cell to transform into an antibody factory and may also reinforce T-cell activity against the same target. In a third role, B cells can secrete cytokines that can inflame or suppress immune activity. The session talks addressed all three roles.
Healthier at the source
Multiple autoimmune diseases seem to run in certain susceptible families, but when it comes to autoreactive B cells, MS differs in a subtle way from type 1 diabetes and rheumatoid arthritis, according to Eric Meffre, Ph.D., an immunobiologist at Yale University in New Haven, Connecticut, Meffre studies the repertoire of B-cell receptors to learn how B cells tolerate a body's own antigens and what goes wrong in autoimmune diseases at two key quality-control checkpoints that shape the destiny of freshly minted B cells.
After birth and throughout life, the bone marrow serves not only as a nursery for constantly newborn B cells that randomly generate millions of unique antigen receptors but also as a quality-control site to eliminate the inevitable self-reactive B cells in at least three different ways. A second peripheral checkpoint catches autoreactive naive mature B cells just after they escape the bone marrow, studies by Meffre and others suggest.
"Most MS suffers from a specific defect in peripheral tolerance," Meffre said in his talk. "In MS, B cells are not intrinsically faulty, and the defect probably resides in regulatory T cells," which may normally prevent the accumulation of autoreactive B cells in circulation.
In a series of studies, Meffre and colleagues have analyzed the frequency of clones expressing autoreactive antibodies at different stages of B-cell development in untreated people with disease compared with healthy controls. They found evidence for defects in both the central and peripheral tolerance checkpoints in 10 of 10 people with rheumatoid arthritis (Samuels et al., 2005; Menard et al., A&R, 2011) and in 12 of 12 people with type 1 diabetes (Menard et al., JCI, 2011). The same may be true with lupus, according to preliminary findings in an ongoing study, Meffre said.
In contrast, five of seven people with MS (Kinnunen et al., 2013) showed B cells within the range of normal central tolerance, but all seven people had high counts of autoreactive naive B cells, suggesting a problem mainly at the peripheral checkpoint.
"The origin of autoreactive clones may be different in MS," said Meffre, citing genetic evidence. A variation in the protein tyrosine phosphatase PTPN22 gene, for example, allows more autoreactive B cells to survive in the bone marrow of healthy people and is associated with a greatly increased risk for type 1 diabetes and rheumatoid arthritis, but not MS, he said.
The apparently healthier origins of B cells in MS reinforce the potential of rituximab and other B-cell depletion therapies to reset peripheral tolerance in MS, Meffre said.
He also is curious about the effect of rituximab and other B-cell depletion therapies on regulatory T cells in people with MS. For example, after being depleted, do restored B cells change the immune cell conversation and restore peripheral tolerance?
B cells and cytokines
One thing is clear: The effect of rituximab on B cells has changed the conversation of scientists by seemingly challenging the role of antibodies in targeted central nervous system (CNS) myelin destruction, noted Rui Li, M.D., a Ph.D. candidate at McGill University and Montreal Neurological Institute, Canada, in his talk.
"This raised the question, What kind of function, other than antibody production, do B cells...contribute to disease?" Li said.
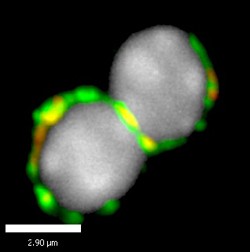
Mouse studies have revealed that B cells can spew proinflammatory cytokines in a newer role called B effector cells. Li looked at what might be happening in people. By staining multiple cytokines simultaneously, he and his colleagues identified a new B-cell subset abnormally increased in blood samples of 20 untreated people with RRMS compared with a matched number of healthy controls.
Li named the B cells for a cytokine they secrete, granulocyte-macrophage colony-stimulating factor. The cells also churn out tumor necrosis factor alpha and interleukin 6, which contribute to exaggerated T-cell responses. Further experiments showed the new subset arises from memory B cells, can be induced by T cells or cytokines and be repressed by B regulatory cells, and enhances innate immune activity. The cells may represent an attractive new therapeutic target in MS, Li and colleagues conclude in the conference abstract.
Anti-B-cell clinical trials
Even after 5 years, the most convincing published evidence implicating B cells in MS remains the original rituximab phase 2 clinical trial (Hauser et al., 2008), said immunologist Andrew Chan, M.D., Ph.D., senior vice president of research biology at Genentech.
A division of the Roche Group, Genentech makes rituximab, a chimeric human–mouse monoclonal antibody that targets the CD20 antigen receptor expressed on all B cells from the time they are suited with antigen receptors in the bone marrow until they convert to short-lived antibody factories known as plasma cells. The drug is approved for B-cell cancers, for rheumatoid arthritis that has failed anti-TNF-alpha therapy, and for a few rare disorders, Chan said. For MS, the company is developing a humanized monoclonal antibody, ocrelizumab, which is in phase 3 clinical testing for RRMS and primary progressive MS. In addition, GlaxoSmithKline is testing a humanized anti-CD20 monoclonal antibody called ofatumumab (Dobson et al., 2011).
Among autoimmune diseases, the best pretrial odds for the effectiveness of rituximab therapy had been for lupus, an autoimmune disease dominated by autoantibodies produced by plasma cells, the end stage of activated B cells. "It failed in lupus—whether by study design or biology is a point of controversy," Chan said. In trials in children with type 1 diabetes, people treated with rituximab partially preserved function of insulin-producing beta cells and demonstrated better control of blood sugar, he added (Pescovitz et al., 2009).
Chan reviewed data of a phase 2 trial of ocrelizumab for people with RRMS, which he noted had been presented at the 2013 meetings of the American Academy of Neurology and the 2013 World Congress on Controversies in Neurology. The findings have not been published. This multicenter randomized trial of 220 people showed that patients treated with ocrelizumab had a rapid reduction in lesions detected by magnetic resonance imaging, the primary endpoint, as well as a lower annualized relapse rate when compared with the control group or patients treated with interferon-beta. Slightly better results came from people in the lower-dose group compared with those in the higher-dose group.
Also interesting, Chan said, was that the results seemed to hold for the three-quarters of participants who continued on an uncontrolled open-label extension of the study, receiving ocrelizumab every 6 months for up to 18 months. The people who had received the experimental treatment were followed-up for another year and a half, with promising results, said Chan, who told MSDF that these data would be presented at ECTRIMS 2013.
Summing up multiple human and animal anti-CD20 studies from Genentech and others, Chan noted that "circulating B cells are the first to depleted and the last to be repleted." Transitional and naive B cells come back first, followed more slowly by memory B cells. Some B-cell niches, such as the synovium of people with rheumatoid arthritis, are not fully depleted, although tissue-specific B cells are readily zapped when they move into circulation, he said. In response to a question from Amit Bar-Or, M.D., a neurologist and immunologist at the Montreal Neurological Institute in Canada, about how the peripheral depletion might affect the B-cell-rich environment of the CNS in MS, Chan replied that the data are less clear here.
"The investigations you and others are doing to image B cells in the brain pre- and postimmunomodulation therapy will be important," he told Bar-Or, who is a scientific advisory board member of the Accelerated Cure Project, the parent organization of MSDF. Bar-Or will be speaking at the ECTRIMS 2013 B-cell session.
Anti-CD20 acts in multiple ways, Chan speculated. Given the multiple roles by which B cells contribute to disease, interfering with them might have distinctive results in different autoimmune diseases beyond just antibodies. For MS, "if you asked me 2 years ago, I would have said the major mechanism is the ability of B cells to talk to other immune components, such as dendritic cells and T cells," he said. However, a recent report that about half of people with MS have antibodies to the KIR4.1 potassium channel expressed in glial cells may provide an additional mechanism by which B-cell depletion may provide benefit in MS (Srivastava et al., 2012).
Chan did not discuss safety and adverse effects. Several researchers have expressed concern about the safety and adverse effects of B-cell depletion therapy. In human testing of rituximab and other monoclonal antibodies for autoimmune diseases, studies have reported an infrequent adverse effect, progressive multifocal leukoencephalopathy (Tavazzi et al., 2011), which is also a serious but rare effect of the approved MS monoclonal antibody, natalizumab.
New autoreactive B-cell pathway
In her talk, Mridu Acharya, Ph.D., a postdoctoral fellow at Massachusetts General Hospital in Boston, described a new pathway by which an uncommon population of B cells regulates autoreactive responses in mice. Acharya studied a rare set of B1 and marginal zone (MZ) B cells tucked away in the spleen and other tissues, which are sometimes called "innate-like" for their rapid and T-cell-independent response. Acharya observed that mice lacking a sticky surface molecule called alphaV integrin had activated B1 and MZ cells and carried more autoantibodies than wild-type mice.
On further investigation, she found that alphaV subdues another surface molecule called toll-like receptor 9 (TLR9), which normally binds to bacterial DNA but may also react to self-DNA found in a body's own dead cell debris. AlphaV may escort TLR9 inside the cell to the protein scrap heap, and the oversight may block the quick and innate-like reaction of B1 and MZ cells to a body's own apoptotic flotsam. The studies are directly relevant to B-cell activation in mouse models of lupus, but Acharya is interested in extending her studies to an experimental autoimmune encephalomyelitis (EAE) mouse model of MS.
"Our hypothesis is that stimulated TLR9 normally goes to a compartment inside the cytoplasm of the B cells, where signaling is degraded," Acharya said. Without AlphaV, TLR9 signaling may stay on and stimulate B cells to respond to the body's own tissues, she speculated.
B cells in the brain
In MS, scientists believe myelin-specific CD4+ T cells enter the brain and spinal cord on a mission to attack the fatty neuron sheathing. But once there, Goverman said, mouse studies she and others performed by have shown that T cells must be reactivated by an antigen-presenting cell or they leave. Reactivation of T cells "licenses them to start doing their job, which may be to directly kill cells that present myelin antigen or to secrete cytokines that trigger inflammation," she told MSDF. "The cytokines act by weakening the blood–brain barrier and attracting more T cells and other immune cells into the CNS."
Several years ago, Goverman and colleagues reported that T cells responded to two epitopes of myelin antigen (Stromnes et al., 2008) in an EAE mouse model. One epitope stimulated high numbers of effector T cells expressing the inflammatory cytokine Th17, and the other roused T-helper 1 (Th1) cells to the area. The relative abundance of the two types of T cells infiltrating the CNS groups appeared to be key: If Th17 cells equaled or outnumbered Th1 cells, inflammation flared in the brain, she said, but if Th1 cells dominated, inflammation was largely restricted to the spinal cord.
The rituximab study (Hauser et al., 2008) led Goverman to look at whether there is a role for B cells in reactivating T cells within the CNS in EAE mouse models. "If B cells influenced how many Th1 and Th17 cells were reactivated," she reasoned, "they may determine whether inflammation targets the brain or the spinal cord. While B cells are known to be antigen-presenting cells in lymphoid tissues, no one had yet determined whether B cells function as antigen-presenting cells within the CNS itself." Animal studies have implicated a number of roles for B cells, including both pathogenic and regulatory roles, depending on the mouse strain and antigen used to induce EAE (Simmons et al., 2013). "There is controversy in animal models," she said. "B cells are clearly important in MS and probably can do many things."
Using a passive EAE mouse model (Stromnes et al., 2006) and mice genetically engineered to lack B cells, Goverman and her team investigated whether the presence of B cells affected T-cell reactivation. They found that myelin-specific T cells enter the CNS in equal numbers in both wild-type and B-cell-deficient mice but only increase in number in the wild-type mice. After ruling out proliferation and survival rates, the researchers traced the T-cell increase to greater recruitment in mice that have B cells in the CNS. "We hypothesize that B cells are the critical antigen-presenting cells for the first wave of T cells," Goverman said.
The researchers also found differential activation of Th1 and Th17 cells in mice that lacked B cells after EAE induction. The CNS B cells preferentially promoted reactivation of Th1 compared with Th17 cells, Goverman reported, which caused more brain inflammation in the B-cell-deficient mice.
These studies aim to illuminate why inflammation flares and returns to normal in different inflammatory patterns in people, she said.
Key open questions
- How is the peripheral B-cell tolerance checkpoint malfunctioning in MS, and can it be reset?
- How does anti-CD20 B-cell depletion alter the immune system dynamics to improve the symptoms and pathophysiology of MS in RRMS?
- What effect does anti-CD20 B-cell therapy have on B cells in the CNS?
- Will depleting B cells influence whether lesions focus more in the brain than the spinal cord?
Disclosures
Acharya reported no financial disclosures. Chan is an employee of Genentech Inc. Goverman's work was supported by the National Institutes of Health and the National Multiple Sclerosis Society. Meffre reported funding from the National Institute of Allergy and Infectious Diseases.



Comments
Failed to mention why genentech abandoned rituximab and developed ocrelizumab due to patent expiration. Rituximab Phase 2 completed 2008.
In his talk at the ECTRIMS 2013 meeting last week, Stephen Hauser MD, the University of California, San Francisco neurologist who led the game-changing 2008 NEJM study phase 2 study of rituximab, posed a similar question: Why go to ocrelizumab after such robust RRMS data with rituximab?
In the last year, Hauser said, the emerging data has convinced him that ocrelizumab may be a better match for MS in the long run because of its greater potency and tolerability and reduced immunogenicity. (Because this is all phase 2 data, Hauser said, he is keeping a vigilant eye on potential side effects of the newer experimental anti-B cell compound as it proceeds through clinical testing.)
After the talk, Chan explained that the immunogenicity of rituximab (against the mouse portion of the chimeric antibody) had been anticipated in the MS studies, based on data from early rheumatoid arthritis trials of rituximab and of another older chimeric antibody (Remicade/infliximab, which targets tumor necrosis factor alpha (TNF-α)). Chan said his team at Genentech was developing the humanized ocrelizumab before anyone knew if the anti-CD20 antibodies would work in MS. In his talk, Chan noted that ofatumumab, a human anti-CD20 antibody, is undergoing clinical testing for RRMS by GlaxoSmithKline and Genmab A/S. All three antibodies bind comparable overlapping epitopes of the CD20 antigen receptor, he said.
Hauser, Chan and Bar-Or spoke about selective targeting of B cells at a satellite symposium arranged by F. Hoffmann-La Roche Ltd (http://registration.akm.ch/einsicht.php?XNMASKEN_ID=300&XNKONGRESS_ID=195&XNSPRACHE_ID=2&XNSESSION_ID=15661). Unfortunately, satellite symposia are not included in the extensive ECTRIMS2013 Webcast library (http://www.ectrims-congress.eu/2013/scientific-programme/online-library.html).