CSF Metabolite Analysis May Offer Sensitive Biomarkers for MS
The systematic study of the complement of small-molecule metabolites in the CSF suggests altered energy and phospholipid metabolism in MS and may yield quantitative biomarkers
Systematic study of the complement of small molecule metabolites, known as metabolomics, suggests altered energy and phospholipid metabolism in multiple sclerosis (MS) and may yield quantitative biomarkers in cerebrospinal fluid (CSF).
“Currently, diagnosis of MS is based on clinical criteria including signs and symptoms, magnetic resonance imaging (MRI), lumbar puncture to identify inflammatory proteins, and excluding other disorders; for many patients, this process can take months,” wrote S. N. Reinke of the Department of Medicine at the University of Alberta in Edmonton, Canada, and colleagues (Reinke et al., 2014). “The lack of a single predictive or diagnostic test at most stages of MS disease remains a major obstacle to patient-oriented care.“
Gene expression and environmental stimuli both affect metabolites, resulting in specific molecular signatures of diseases such as MS. The investigators used 800-MHz 1H nuclear magnetic resonance (NMR) spectroscopy of the CSF, which is at the interface between blood and CNS tissue, to detect a variety of metabolites in persons with or without MS. This technique not only offers quantitative results but is also highly reproducible.
The investigators compared levels of 15 metabolites in 15 participants with MS and in 17 without MS. Overall, the profiles suggested changes in energy and phospholipid metabolism in MS. Specifically, participants with MS had higher mean CSF levels of choline, myoinositol, and threonate, but lower mean CSF levels of 3-hydroxybutyrate, citrate, phenylalanine, 2-hydroxyisovalerate, and mannose, than participants without MS (P < 0.05).
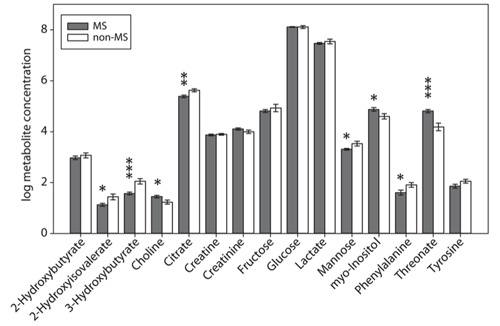
There was a high correlation within the metabolite profiles, so that the samples were significantly clustered into the two clinical groups (MS versus non-MS). The investigators showed this using a statistical technique known as multivariate hierarchical cluster analysis and confirmed the results using principal components analysis.
In other words, each specimen was most metabolically similar to those in the same clinical group, and the profile means differed significantly between the two groups, suggesting the potential for metabolic diagnostic biomarkers of MS.
“CSF metabolomics have the capacity to yield quantitative biomarkers and insights into the pathogenesis of MS,” the study authors wrote.
NMR more useful than HPLC?
Interestingly, high-performance liquid chromatography (HPLC) analysis of CSF from MS and non-MS patients did not reveal any significant differences in amino acid levels between groups. This suggests that NMR is a more useful technique than HPLC to detect metabolites in the CSF of MS patients that could serve as diagnostic biomarkers.
“This study shows that by using higher field strength 1H-NMR spectroscopy, stringent inclusion criteria, and exploratory multivariate data modeling methods, MS and non-MS patients can be discriminated by group with a high level of significance,” the study authors concluded. “While this study requires validation with greater sample sizes, it demonstrates the potential for a metabolomic profile-based diagnostic strategy for multiple sclerosis.”
Key open questions
- How will metabolomic profile analysis assist in the diagnosis of MS and/or in the detection of asymptomatic persons who will develop clinical MS?
- How will metabolomic profile analysis assist in monitoring treatment responses among persons with MS?
- What additional insights into the pathogenesis of MS may metabolomic profile analysis offer?
Disclosures and sources of funding
The study was supported by grants from The Multiple Sclerosis Society of Canada, Alberta Innovates Health Solutions Collaborative Research and Innovation Opportunities, Canadian Institutes of Health Research, the Bud and Lorna Atkin Endowment Fund for MS Research, and the Barrhead-Fort Assiniboine Endowment Fund for MS. One of the study authors receives salary support from Pfizer Canada, another held a Multiple Sclerosis Society of Canada Postdoctoral Fellowship, and a third holds a Canada Research Chair (T1) in Neurological Infection and Immunity. The other authors reported having no financial disclosures.


