Low CD8+ T Cell Counts Found With Dimethyl Fumarate
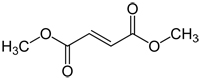
A recent study found that patients taking dimethyl fumarate (Tecfidera) had low counts of CD8+ T cells, though their overall levels of lymphocytes were within the normal range. The findings suggest that physicians may want to monitor specific lymphocyte levels in addition to doing full blood cell counts.
 In November 2014, Biogen Idec confirmed its first case of progressive multifocal leukoencephalopathy (PML), a rare brain infection, in a patient taking dimethyl fumarate (Tecfidera), and complications from the infection resulted in the patient’s death. The news sparked a warning from the U.S. Food and Drug Administration and concern from both patients and physicians about how to prevent another case of PML.
In November 2014, Biogen Idec confirmed its first case of progressive multifocal leukoencephalopathy (PML), a rare brain infection, in a patient taking dimethyl fumarate (Tecfidera), and complications from the infection resulted in the patient’s death. The news sparked a warning from the U.S. Food and Drug Administration and concern from both patients and physicians about how to prevent another case of PML.
Research from the University of California, San Francisco (UCSF), may provide some insight on better monitoring techniques for patients taking dimethyl fumarate (DMF). In a paper published online ahead of print in Neurology, Neuroimmunology and Neuroinflammation (Spencer et al., 2015), researchers followed 14 patients every 3 months for a year and examined levels of leukocyte and lymphocyte subsets including CD3+, CD4+, CD8+ T cells, CD19+ B cells, and CD56+ natural killer cells.
They found that total leukocyte and lymphocyte levels diminished by the 6-month mark and that half the patients had leukocyte levels below the lower limit of normal. While the levels of all the cell subsets dropped over time, the researchers noted a particularly striking decrease in the level of CD8+ T cells, which are primarily involved in responding to viral infection.
PML develops from an opportunistic virus called the John Cunningham virus. DMF comes with a recommendation that physicians take blood cell counts of patients before starting on the drug and annually or as clinically necessary afterward. The safety precautions recommend that physicians consider interrupting treatment if lymphocyte counts decrease below 500 cells/μL in the blood and the low levels persist for 6 months. The label also says patients should stop taking DMF if any symptoms of PML occur, which include “clumsiness; progressive weakness; and visual, speech, and sometimes personality changes,” according to the National Institute of Neurological Disorders and Stroke. The symptoms of PML can also develop slowly over the course of weeks to months.
Typically, cell counts look at the major types of blood cells (red blood cells, lymphocytes, and leukocytes) but do not look at subsets. What the UCSF team found was that patients may have dangerously low levels of cell subsets, like CD8 cells, while still having total leukocyte and lymphocyte counts within the normal range.
“[CD8+ T cells] are the cells that are very important in antiviral immunity,” corresponding author Scott Zamvil, M.D., Ph.D., of UCSF told MSDF. Without the CD8+ T cells, the JC virus that leads to PML may be more able to infiltrate the body while the immune system has its guard down. But due to the small sample size and the relative short duration of the study, Zamvil said the results are not yet definitive. “So we need more investigation. These results are cautionary.”
Zamvil also said that the investigators did not take biopsies of the brain or lymph nodes, which may have different cell levels that could affect a patient’s susceptibility to or protection from PML. But due to the nature of the results, Zamvil told MSDF that he and his colleagues felt it important to get their data out there so that clinicians can make use of it.
Key open questions
- How can these results be incorporated into the safety information for DMF?
- What is the most efficient way to monitor for changes to leukocyte and lymphocyte subtypes?
Disclosures and sources of funding
The researchers did not report any targeted funding for this study.
Among the study’s authors, C. M. Spencer reported no disclosures. E. C. Crabtree-Hartman has consulted for Teva, Novartis, and Biogen and has been on the speakers’ bureau for Teva Neuroscience and Biogen. K. Lehmann-Horn received research support from the Deutsche Forschungsgemeinschaft and U.S. National Multiple Sclerosis Society. B. A. C. Cree is an editor for Annals of Neurology; has consulted for AbbVie, Biogen Idec, EMD Serono, Genzyme, MedImmune, Novartis, Sanofi Aventis, and Teva Neurosciences; received research support from Acorda, Avanir, Biogen Idec, EMD Serono, Hoffmann-La Roche, MedImmune, Novartis, and Teva Neurosciences; and was an expert consultant for Biogen Idec. S. S. Zamvil received honoraria for serving on the data and safety monitoring boards from BioMS, Teva Pharmaceuticals, and Eli Lilly; is the deputy editor for Neurology: Neuroimmunology & Neuroinflammation; has a patent pending for aquaporin-4 peptides and methods for using the same; received speaker honoraria from Biogen Idec, Teva Neuroscience, and Genzyme; has consulted for Biogen Idec, Teva Neuroscience, EMD Serono, Genzyme, and Novartis; is on the speakers’ bureau for Advanced Health Media and Biogen Idec; and received research support from NIH, the National Multiple Sclerosis Society, the Maisin Foundation, and the Guthy-Jackson Charitable Foundation.


